New compounds target and kill brain cancer cells with low X-ray dose
Mice with brain tumours survived twice as long after being treated with the compounds.
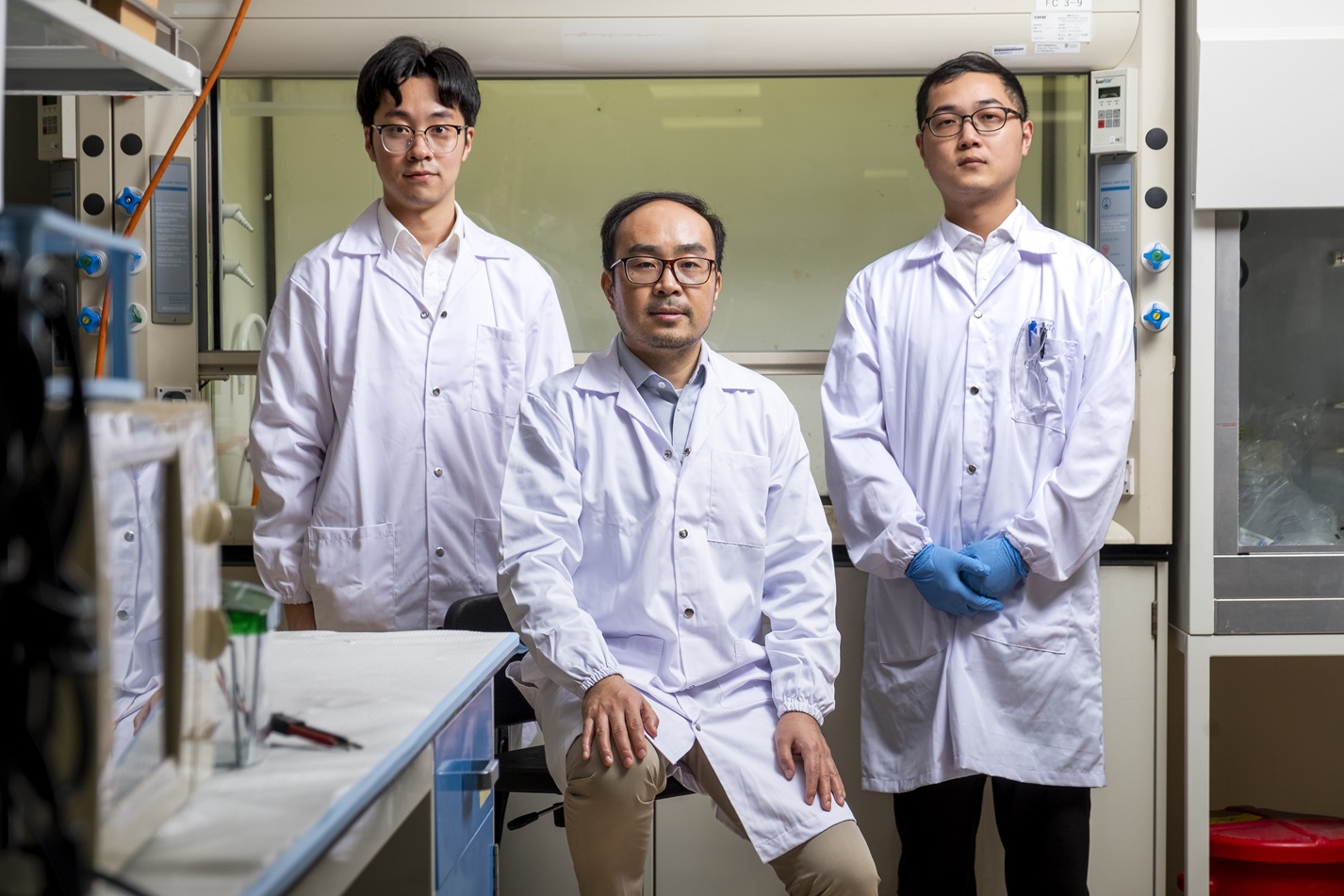
(From left) PhD student Xu Cheng, Prof Pu Kanyi and research fellow Dr Huang Jingsheng from NTU Singapore’s School of Chemistry, Chemical Engineering and Biotechnology are involved in developing new compounds that precisely kill brain tumour cells. (Credit: NTU Singapore)
Researchers led by Nanyang Technological University, Singapore (NTU Singapore) have developed a new and precise way to treat the most common type of brain cancer using a substantially lower dose of X-rays than existing radiation treatments.
The method has been shown to curb the growth of brain tumours in mice, which paves the way for future clinical applications in humans.
Every year, more than 300,000 people are diagnosed globally with glioblastoma, the most common brain cancer among adults. The cancer starts as a growth of brain cells and, if not treated, quickly spreads through the brain. On average, patients diagnosed with glioblastoma survive for about one and a half years.
One way to treat it is by using radiation like X-rays to kill the cancer cells. However, radiotherapy can accidentally damage healthy cells near the tumour, leading to side effects such as nausea, hair loss and memory problems.
Radiodynamic therapy is a more recent treatment option under development, in which a patient is injected with specially made compounds that create cancer-killing free radicals when X-rays activate them. The dose of X-rays patients receive to activate the compounds is lower, about 20 to 30 per cent of the dose for conventional radiotherapy.
However, the anti-cancer compounds used in radiodynamic therapy, which contain heavy metals, do not target cancer cells accurately. They find their way into healthy cells and can be activated if they are close to where the patient receives the X-rays, leading to damage in the healthy cells.
Now, new research led by NTU’s Prof Pu Kanyi, from the School of Chemistry, Chemical Engineering and Biotechnology, holds promise in addressing these problems to make radiation treatment for glioblastoma safer. The study was published in September 2023 in Nature Materials.
Precision cancer killing

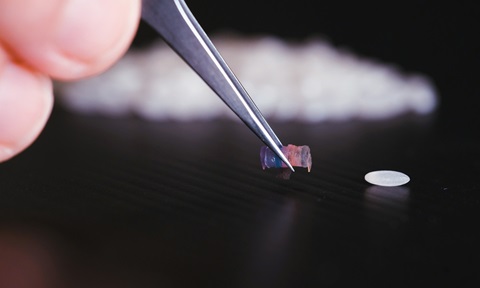
Research fellow Dr Huang Jingsheng from NTU Singapore’s School of Chemistry, Chemical Engineering and Biotechnology preparing new anti-brain cancer compounds in a fume hood. A silica column was used to get a purified form of the compounds (yellow liquid in flask). (Credit: NTU Singapore)
At the heart of Prof Pu’s advance is a novel compound developed by his team known as a molecular radio afterglow dynamic probe or “MRAP”. It comprises biochemicals and iodine and no heavy metals.
In experiments with mice that had brain cancer, the MRAPs were injected directly into the animals’ tumours, followed by X-rays at the same location. The X-ray dosage was equivalent to more than six times lower than the amount administered in existing radiodynamic therapy methods.
The MRAPs in the tumours absorb the X-ray radiation and become energised, unleashing cancer-killing free radicals only when they encounter a specific enzyme produced in abnormally large quantities by brain tumour cells.
In their experiments, the NTU team observed that the MRAPs did not produce free radicals in normal cells, creating no side effects. By contrast, traditional radiodynamic therapy compounds are not as “smart”, and their anti-cancer functions can become activated even in healthy cells.
As a result, the side effects of using MRAPs in humans are expected to be lower than other types of radiation treatment.
After treatment with MRAPs, the brain tumours in the mice stopped growing, and these mice survived twice as long as untreated mice – 76 days compared with 37.
The animals also showed no sign of tissue damage nor apparent weight loss after being treated with MRAPs. The compounds were eventually passed out through urine and faeces.
“We used very low dosages of X-rays and cancer-killing MRAPs. Also, the anti-cancer compounds were active only in the brain tumour and not healthy cells,” said Prof Pu. “So, we expect our treatment method to be safer and have fewer side effects than existing ones.”
A patent has been filed on the MRAPs, and Prof Pu’s team is in discussions with potential investors who are keen on the research.

PhD student Xu Cheng from NTU Singapore’s School of Chemistry, Chemical Engineering and Biotechnology checking an X-ray machine for radiation leakage. The properties of new anti-brain cancer compounds were determined by energising them with X-rays in the machine. (Credit: NTU Singapore)
The findings from Prof Pu’s team “represent an important advance in combining X-rays and light to detect and treat microtumours”, said Professor Marc Vendrell from The University of Edinburgh in Scotland, the United Kingdom, who was not involved in the study.
Prof Vendrell, who develops chemical probes targeting cancer and inflammation for translational imaging studies in the clinic, added that the research “opens new avenues for the precise elimination of tumour cells in cancer patients”.
“The results are very promising in that the treatment can be very effective against small tumours and with safe dosages of radiation,” he said. “The next steps will be to evaluate the safety and efficacy of these treatments in larger pre-clinical models and, subsequently, first-in-human studies.”
In the future, Prof Pu’s team plans to improve the MRAP’s ability to target cancer cells and add cancer-curbing functions such as immunotherapeutic abilities that would help activate the immune system to destroy cancer cells and aid the body in fighting cancer recurrence.
Earlier experiments by the team, published in December 2022 in Nature Biomedical Engineering, showed that in mice with cancer, another type of anti-cancer compound the scientists developed staved off new cancer cells introduced into the animals.
This was linked to the activation of the mice’s cancer-fighting immune cells. But instead of X-rays, these anti-cancer compounds were energised by ultrasound.

New anti-brain cancer compounds in a foil-covered tube loaded in an X-ray machine to determine their properties by energising them with X-rays. (Credit: NTU Singapore)
---
Details of the study can be found in “Molecular radio afterglow probes for cancer radiodynamic theranostics” in Nature Materials (2023) and “Nanoparticles with ultrasound-induced afterglow luminescence for tumour-specific theranostics” in Nature Biomedical Engineering (2022).

-and-dr-dorrain-low-from-ntu-singapore's-lkcmedicine.tmb-listing.jpg?Culture=en&sfvrsn=b389b500_1)

.tmb-listing.jpg?Culture=en&sfvrsn=82921582_1)
.tmb-listing.jpg?Culture=en&sfvrsn=9b7345be_1)