Gist of the jab
As vaccines to prevent COVID-19 roll out, we ask Assoc Prof Luo Dahai, an infectious disease expert at NTU’s Lee Kong Chian School of Medicine about the jab, including how it works, its effectiveness and safety, and whether you need it.

What are the main types of COVID-19 vaccines?
As of mid-June, there are eighteen approved COVID-19 vaccines worldwide. So far, the vaccines developed by Pfizer-BioNTech and Moderna have been approved by the Health Sciences Authority for use in Singapore. All the vaccines prompt our bodies to recognise the virus that causes COVID-19 and prevent us from becoming severely ill with the disease. The main difference between them is how the vaccine presents the viral antigens – substances from the virus that stimulate an infection-fighting immune response. Inactivated virus and mRNA vaccines are two of the main types of COVID-19 vaccines available.
How do the inactivated virus COVID-19 vaccines work?
Vaccines such as CoronaVac from Sinovac and the Sinopharm vaccine use dead coronavirus to train the body’s immune system to respond to the actual virus, which is how conventional vaccines immunise us against infectious diseases. These vaccines retain the viral antigens and trigger the correct immune response without causing infection. You can think of the dead viruses as target practice for your immune system so that it recognises and attacks the virus when it comes along.
What are mRNA vaccines and how do they work?
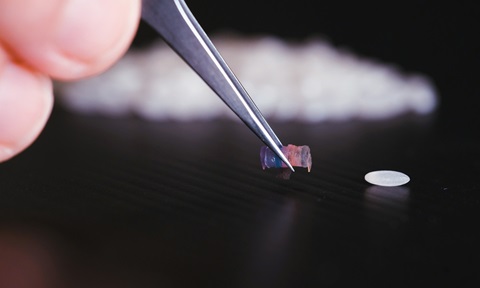
mRNA vaccines such as the ones from Pfizer-BioNTech and Moderna were developed during the pandemic. They use messenger RNA (mRNA) – genetic instructions that our cells read – to make viral proteins present on the outer surface of the coronavirus. Our immune system recognises these proteins as foreign invaders and mount a defence against it when the actual virus is encountered. Our bodies are not exposed to the actual virus but are trained to fight it.
There have been some unwarranted concerns about whether the mRNA in the vaccines will alter our DNA. The mRNA does not combine with DNA in our cells and breaks down quickly and completely after the viral proteins are produced. Hence, it will not change our DNA in any way.
It usually takes 10 years or more to develop a vaccine. With the COVID-19 vaccines developed and approved in such a short time, how can we be sure they are safe and effective?
Previous research on similar viruses and unprecedented cooperation between researchers, governments and regulators accelerated the development of the COVID-19 vaccines. Clinical trials were completed quickly but were rigorously conducted, following the same protocols used to test commercial vaccines against other pathogens.
The coronavirus vaccines are also approved by health authorities based on the same stringent criteria used to evaluate other vaccines. The results of the clinical trials show the vaccines are safe and effective.
There have been a few cases of allergic reactions to the vaccines and some people have developed blood clots after being vaccinated. Should I be worried?
As with any type of vaccine, there will always be some cases of mostly mild but possibly severe allergic reactions or side effects. A small risk of adverse reactions is unavoidable, given that populations are diverse in many ways.
But there’s no need to be overly worried about the possibility of a severe reaction to the COVID-19 vaccines. Vulnerable individuals such as pregnant women, patients with chronic health conditions and those with weakened immune systems should seek their doctor’s advice before considering vaccination.
That said, the benefits of vaccination greatly outweigh its risks and everyone who is eligible for the vaccine should get vaccinated when they can.
There have been a few cases of people getting infected even after they were vaccinated. Does this mean that the vaccines are not effective?
Like all vaccines, the COVID-19 vaccines reduce the likelihood that an infected person will become severely ill with the disease. However, everyone’s immune system is unique and will not respond to the vaccine in the same way. Vaccinated persons who are not able to mount a strong immune response to the vaccine can still be infected and fall ill. While no vaccine is foolproof, vaccination will help lower the risk of infection and severe disease.
As such, people should consider getting vaccinated when it is their turn to do so.
Since most coronavirus patients recover from the infection and possibly develop immunity to it, what is the main advantage of being vaccinated?
Besides protecting yourself from illness, getting vaccinated against COVID-19 will prevent the virus from spreading to others in the community. Remember that the elderly and those with chronic health conditions or weakened immune systems are more likely to become critically ill with COVID-19. When most of the population is protected against the disease, the spread of the virus is reduced and these individuals as well as other unvaccinated people are less likely to be infected. This prevents COVID-19 infections from spiralling out of control and burdening healthcare systems.
Are the vaccines effective against new coronavirus variants such as those detected in UK, South Africa and India?
Some laboratory-based studies suggest the currently approved COVID-19 vaccines provide some protection against these variants as the vaccines trigger a broad immune response to the virus. A study has found that the Pfizer-BioNTech vaccine was 88 per cent effective against the Delta variant and 93 per cent effective against the Alpha variant. More thorough clinical studies are ongoing to draw more reliable conclusions.
Will vaccination against COVID-19 help us get back to pre-pandemic life?
Perhaps. Vaccination will certainly help reduce the spread of the virus so that we can resume our lives. However, several questions remain about how long the immunity from the vaccine lasts or if it can prevent asymptomatic patients from transmitting the virus. It may be a while before we’re back to the old normal. But still, it is better for as many of us to be vaccinated as possible.
New strains of the virus have also emerged. Nevertheless, a successful vaccination campaign will slow down the spread of the virus and help prevent resistant strains from emerging.


.tmb-listing.jpg?Culture=en&sfvrsn=82921582_1)

.tmb-listing.jpg?Culture=en&sfvrsn=ba129532_1)

